Specialist care for jaw joint pain, clicking, and movement problems
TMJ Management and Surgery Sydney
The Temporomandibular Joint (TMJ) plays an essential role in talking, chewing, and daily function. Problems with this joint often called Temporomandibular Disorders (TMD) can cause pain, stiffness, or restricted movement. For many patients, non-surgical options provide relief, while others may require surgery.
With more than 15 years of specialist practice, Dr Kristian van Mourik provides comprehensive TMJ management at clinics in Bondi Junction and Lindfield.


Our practice provides a wide scope of oral and maxillofacial surgery in Sydney, built on more than 15 years of specialist experience. With two established clinics and a patient-first approach, we focus on careful planning, clear communication, and safe surgical care. Learn more about our team and history in the link below
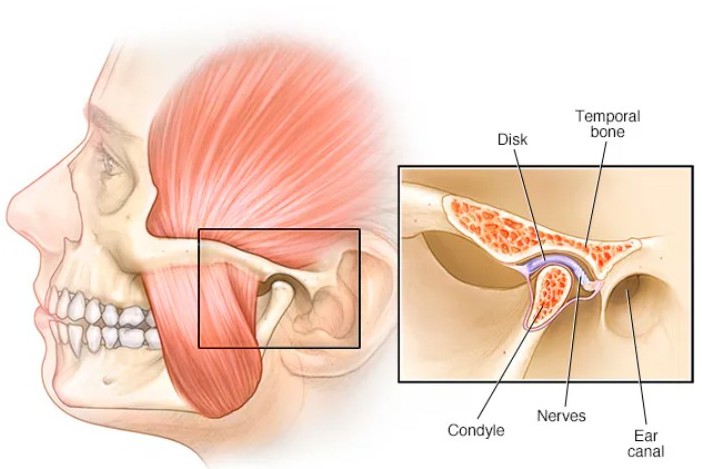
What is the TMJ Joint?
Your temporomandibular joint (TMJ) connects your lower jaw to your skull on each side of your head. It’s one of the most complex joints in the body, allowing you to talk, chew, and yawn comfortably. The joint connects the mandibular condyle (jawbone) to the temporal bone (skull).
TMJ disorders can occur due to arthritis, injury, teeth grinding or clenching (bruxism), or a misaligned bite. While most TMJ problems can be treated without surgery, about 5% of people with severe cases may need a surgical procedure.
What are the Signs of TMJ Disorder?
TMJ disorders can affect patients in different ways, ranging from mild discomfort to significant disruption of daily activities. Common symptoms include:
Jaw pain and tenderness
Pain is often felt near the ear or along the jawline, and may worsen when chewing, speaking, or yawning. Some patients also report pain spreading to the temples, face, or neck.
Clicking, popping, or grinding
Noises from the joint when opening or closing the mouth can be harmless, but when combined with pain or limited movement, they may indicate underlying dysfunction.
Restricted jaw movement
Some patients struggle to open their mouths fully, while others experience the jaw “locking” open or closed, making eating and speaking difficult.
Headaches and neck pain
Muscle strain around the jaw and joint can radiate into the head, neck, and shoulders, leading to tension headaches or persistent stiffness.
Bite or chewing difficulties
An uneven bite or joint strain can cause pain when eating, making certain foods difficult to chew and limiting diet choices.
How to Diagnose TMJ Disorders
Dr van Mourik will begin with a thorough clinical examination to assess your jaw movement, bite, and areas of tenderness.
You may also need diagnostic imaging such as:
- Dental X-rays – to evaluate teeth and jaw alignment
- CT scans – to show detailed bone structure
- MRI scans – to reveal issues with the TMJ disc or soft tissues
In some cases, a TMJ arthroscopy is performed for diagnosis. This involves inserting a fine camera (arthroscope) into the joint space to view and assess the structures directly. TMJ arthroscopy can also be used therapeutically to remove inflamed tissue or scar tissue, improving jaw movement and reducing pain.

What are the Treatment Options for TMJ Pain?
TMJ management starts with a thorough assessment using clinical examination and advanced imaging such as CT or MRI scans. These provide detailed insight into the joint, muscles, and surrounding structures, allowing treatment to be tailored to each patient.
Conservative management options include:
- Self-care and lifestyle changes: Apply heat or ice, avoid gum chewing and extreme jaw movements, practise relaxed jaw posture, and manage stress.
- Medications: Pain relievers, anti-inflammatories, muscle relaxants, or low-dose tricyclic antidepressants may reduce pain and muscle tension.
- Oral splints or mouthguards: Worn at night to reduce grinding and jaw strain.
- Physiotherapy: Jaw stretching and strengthening exercises, ultrasound therapy, or TENS (transcutaneous electrical nerve stimulation).
- Counselling: Addresses habits that worsen TMJ pain, such as clenching or nail-biting.
- Injections: Corticosteroid or botulinum toxin (Botox®) injections may provide relief by reducing inflammation and muscle tension. These effects are usually noticeable within 2 weeks.
Surgical options may be considered if symptoms persist:
- Arthrocentesis (Joint Washout)
A minimally invasive procedure that flushes the joint using sterile fluid to remove debris and inflammatory byproducts. It helps reduce pain and improve jaw mobility.
- Arthroscopy
A small incision is made in front of the ear and a fine arthroscope (camera) is inserted to view the joint. Damaged tissue can be repaired, and inflammation can be treated. This technique has fewer risks and a shorter recovery time than open surgery.
- Arthrotomy (Open-Joint Surgery)
An open approach allows the surgeon to visually examine the joint and perform repairs or tissue biopsies. This option is typically for more complex TMJ conditions.
- Modified Condylotomy
This procedure addresses the TMJ indirectly through surgery on the lower jawbone (mandible), rather than inside the joint itself, to ease pain and locking.
- Total Joint Replacement
When other treatments fail, the damaged TMJ may be replaced with a custom metal prosthesis. This is a major surgery performed under general anaesthetic in a private hospital, with a longer recovery period.
How long does treatment take?
Minimally invasive treatments such as arthrocentesis are usually performed as day procedures, with recovery in just a few days. More complex surgeries, such as open joint surgery, require longer healing times and follow-up care.
Will I be awake during treatment?
Comfort is prioritised for every patient. Depending on the type of procedure, local anaesthetic, intravenous sedation, or general anaesthesia may be used.
When is TMJ Surgery Recommended?
Surgery is generally only considered when non-surgical treatments have not relieved symptoms. It may be recommended when:
- Pain continues to interfere with daily activities despite conservative management.
- The jaw locks open or closed, restricting normal function.
- Clicking, popping, or grinding noises are associated with limited movement or discomfort.
- Imaging shows structural changes such as displaced discs or joint degeneration.
- TMJ problems are significantly impacting quality of life, such as eating, speaking, or sleeping.
Every case is assessed individually. Risks, benefits, and alternatives are discussed thoroughly so patients can make an informed decision.
Recovery After TMJ Surgery
Recovery time varies depending on the type of procedure performed. Most patients experience mild discomfort and can gradually return to normal activities over the following weeks.
Hospital Stay
- Arthroscopy or Arthrocentesis: Usually performed as day surgery.
- Complex Procedures (e.g. Joint Replacement): May require a 3–4 day hospital stay.
Pain Management
- Mild Procedures: Pain is generally managed with Nurofen® or Panadeine Forte®.
- Joint Replacement: IV pain relief is provided for the first 48 hours, followed by oral medication.
Time Off Work or School
- Arthroscopy, Arthrocentesis, or Arthrotomy: Allow approximately 3 days off.
- Joint Replacement: Plan for around 2 weeks off.
Diet and Wound Care
- Soft Diet: Continue for 3–4 weeks post-surgery.
- Stitches: Dissolving stitches usually disappear within 1–2 weeks.
Follow-Up Visits
- Regular reviews ensure proper healing and jaw function
Recovery After TMJ Botox Injections
Recovery after TMJ Botox injections is minimal. Most patients can return to normal activities immediately, though mild swelling or redness at the injection site is common.
Activity and Position
- Remain upright for 4 hours after treatment.
Avoid for 24 Hours
- Alcohol or exercise (including swimming).
- Nurofen® or other anti-inflammatory medication.
- Touching or rubbing the treated area.
- Applying makeup, sunscreen, or skincare to the site.
- Direct sunlight exposure.
Avoid for 1 Week
- Facial massages, waxing, or other beauty treatments.
Possible Temporary Effects
- Mild swelling, redness, bruising, or tenderness.
- Headache or fatigue lasting 1–2 days.
Why Seeing an Oral and Maxillofacial Surgeon Matters
TMJ disorders often involve a mix of joint, muscle, and bite-related issues. Oral & Maxillofacial Surgeons are uniquely trained as doctors, dentists, and specialist surgeons — giving them the expertise to diagnose and treat these complex conditions.
Benefits of specialist care:
Expert precision: Procedures performed with advanced anatomical knowledge
Faster recovery: Less trauma to surrounding tissues
Lower risk: Reduced chance of infection or joint complications
Comprehensive care: Surgeons can manage any issues that arise
Long-term results: Guided by the latest medical and dental research
Trust an Oral & Maxillofacial Surgeon for accurate diagnosis, effective treatment, and lasting relief from TMJ pain.

Meet Dr Kristian van Mourik
Dr Kristian van Mourik is a fully qualified Oral & Maxillofacial Surgeon with more than 15 years of specialist practice in Sydney. He holds dual degrees in medicine and dentistry, supported by extensive surgical training, making him one of the few surgeons in Australia with this level of expertise.
Academic background includes:
- Bachelor of Biomedicine – Monash University
- Bachelor of Dentistry with Honours – University of Sydney
- Bachelor of Medicine / Bachelor of Surgery – University of Sydney
His practice covers the full scope of oral and maxillofacial surgery, including TMJ disorders, corrective jaw surgery, wisdom tooth removal, dental implants, trauma surgery, and oral pathology. Dr van Mourik is registered with both the Medical Board of Australia and the Dental Board of Australia as a specialist Oral & Maxillofacial Surgeon.

Areas We Service for TMJ Management and Surgery
TMJ management and surgery available across Sydney’s Eastern Suburbs and North Shore.
- Bondi
- Bronte
- Clovelly
- Coogee
- Randwick
- Paddington
- Woollahra
- Double Bay
- Bellevue Hill
- Tamarama
- Waverley
- Surrounding Eastern Suburbs
- Roseville
- Chatswood
- Killara
- Gordon
- Pymble
- Turramurra
- St Ives
- Wahroonga
- Hornsby
- Willoughby
- Castle Cove
- Other North Shore suburbs
TMJ FAQs Sydney
Do all TMJ problems require surgery?
No. Most TMJ conditions are managed with conservative care. Surgery is only recommended when symptoms persist and interfere with quality of life.
What is recovery like after TMJ surgery?
Recovery depends on the procedure. Minimally invasive options often require only a few days of downtime, while open surgery involves a longer recovery period.
Are TMJ disorders common in Sydney?
Yes. Many adults across Sydney experience TMJ-related symptoms such as jaw pain, clicking, or stiffness, particularly those who grind or clench their teeth due to stress.
Can stress cause TMJ problems?
Yes. Stress-related clenching and grinding are among the most common causes of TMJ issues. Managing stress is often part of treatment.
Where is TMJ surgery performed?
Procedures are carried out in accredited private hospitals, supported by specialist anaesthetists and surgical teams.
Our Sydney Clinics

Bondi Junction
Located in the heart of the Eastern Suburbs, our Bondi Junction clinic is easily accessible by train, bus, and nearby parking.

Lindfield
Conveniently positioned on the North Shore, our Lindfield clinic is close to public transport and offers parking options nearby.
