Specialist surgical care for patients with obstructive sleep apnoea (OSA).
Sleep Apnoea Surgery Sydney
Sleep apnoea surgery in Sydney designed to improve breathing, reduce snoring, and enhance sleep quality through advanced oral and maxillofacial care.
With more than 15 years of specialist experience, Dr Kristian van Mourik provides advanced sleep apnoea surgery at clinics in Bondi Junction and Lindfield.


Our practice offers comprehensive oral and maxillofacial surgery in Sydney, backed by more than 15 years of specialist training and clinical experience. With two established clinics and a patient-centred approach, we focus on careful planning, precise surgical technique, and clear communication.
Dr van Mourik works closely with sleep physicians, ENT specialists, and orthodontists to deliver effective, evidence-based treatment for obstructive sleep apnoea (OSA).
Learn more about our practice, our team, and our approach to surgical excellence in the link below.
Symptoms and problems caused by obstructive sleep aponea
Obstructive sleep apnoea can significantly affect your quality of sleep and overall health. Common symptoms to watch for include:
Excessive daytime sleepiness
Interrupted sleep can cause persistent fatigue, making it difficult to stay awake, concentrate, or perform daily tasks safely especially when driving or working.
Loud or frequent snoring
Snoring is one of the most noticeable signs of airway obstruction. It occurs when airflow is partially blocked, causing vibration of soft tissues in the throat.
Night awakenings accompanied by difficulty breathing
Episodes of breathing pauses often cause patients to wake abruptly, sometimes gasping or choking. These interruptions can occur dozens of times each night.
Rise in blood pressure, increasing risk of heart attack and stroke
Frequent drops in oxygen levels place stress on the cardiovascular system, leading to elevated blood pressure and greater risk of serious heart conditions.
Waking up with a dry mouth or sore throat
Mouth breathing during sleep, often due to airway restriction, can cause dryness, soreness, or discomfort upon waking.
Difficulty concentrating during the day
Poor sleep quality reduces mental clarity and memory, leading to decreased productivity and increased irritability.
Morning headaches
Low oxygen levels and disrupted sleep patterns can contribute to headaches or a heavy, foggy feeling in the morning.
Nighttime sweating
Repeated arousals during sleep trigger the body’s stress response, which may cause sweating or restlessness overnight.
Depression
Long-term sleep disruption can affect mood-regulating hormones, contributing to symptoms of anxiety, low motivation, and depression.
What is obstructive sleep aponea (OSA)?
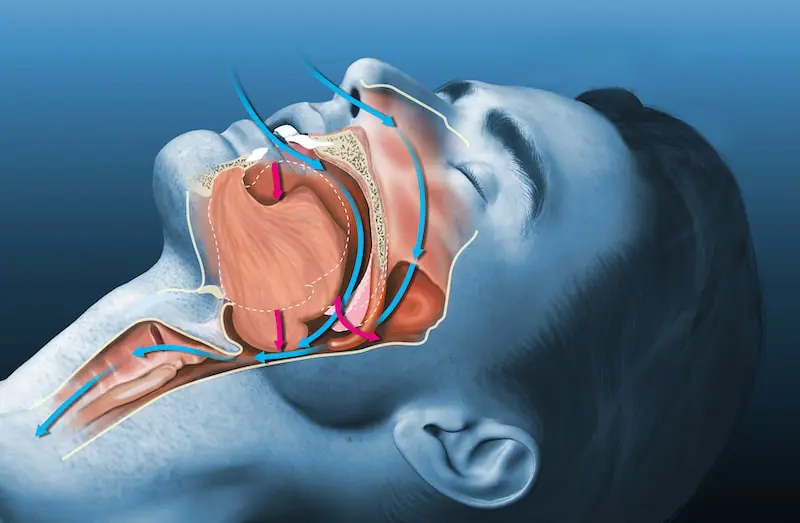
Obstructive sleep apnoea (OSA) is a common sleep disorder where the airway at the back of the throat collapses during sleep, causing repeated pauses in breathing. This can lead to loud snoring, poor sleep, high blood pressure, and increased risk of heart problems. Effective treatments include CPAP therapy, oral appliances, and, in some cases, surgery.
Do I need surgery for OSA?
Surgery for obstructive sleep apnoea isn’t the first treatment option, but it may be considered if other treatments haven’t worked or aren’t suitable for you. You may benefit from seeking a surgical opinion if:
- Your child has been diagnosed with OSA.
- You’re an adult who cannot tolerate CPAP or an oral appliance.
- You have certain anatomical factors, such as large tonsils or malaligned top and bottom jaws that make CPAP less effective.
- You don’t want to wear a CPAP device (though it’s strongly recommended to try it first).
Surgery is only considered after conservative treatments have failed. Before recommending surgery, a specialist, usually an Ear, Nose and Throat (ENT) surgeon or an Oral and Maxillofacial Surgeon , will conduct a series of tests to determine if surgery is likely to help.

Types of Surgery for Obstructive Sleep Apnoea (OSA)
Adults with OSA may need surgery on the nose, upper airway, lower airway, or jaws. Treatment is personalised, with the sleep specialist and oral and maxillofacial surgeon working together to plan the best approach for your anatomy and symptoms. In some cases, a multi-stage treatment plan may be recommended.
Maxillomandibular Advancement (MMA)
Maxillomandibular Advancement (MMA) Most effective surgical option for OSA, with success rates comparable to CPAP.
- This surgery moves both the upper and lower jaws forward to open the airway at the back of the throat, helping prevent blockages during sleep.
- Traditionally performed after soft tissue surgery, but may be a primary procedure
- Performed by an oral and maxillofacial surgeon, a highly specialised surgeon with both medical and dental qualifications.
Rapid maxillary expansion (RME)
- Rapid Maxillary Expansion (RME) widens the upper jaw to increase airway space at the back of the mouth.
- Helps prevent the throat from collapsing during sleep, reducing pauses in breathing and improving oxygen levels.
- Most effective in children, helping prevent long-term complications from sleep apnoea.
- Performed by an oral and maxillofacial surgeon, a highly specialised surgeon with both medical and dental qualifications.
Nasal Surgery
- Nasal obstruction can worsen OSA or make treatments like CPAP less effective.
- Surgical options include:
- Septoplasty (correcting a deviated septum)
- Turbinate reduction
- Removal of nasal polyps
- Sinus surgery or rhinoplasty
- Surgery improves airflow and may make CPAP easier to use.
Upper Throat Surgery
- Tonsillectomy may help patients with enlarged tonsils.
- Modified UPPP (Uvulopalatopharyngoplasty) repositions the palate and throat muscles forward to open the airway.
- Often combined with other upper airway procedures for best results.
Lower Throat Surgery
- Obstruction at the base of the tongue can block the airway during sleep.
- Options include:
- Radiofrequency reduction to shrink tongue tissue
- Surgical removal of excess tissue
- Usually combined with other throat or palate surgeries.
Weight loss surgery
- Reduces excess fat in the tongue, neck, and throat, helping to open the airway.
- May improve or resolve OSA symptoms in some patients.
What Does surgery for sleep aponea involve?
Here is an overview of the preparation and procedure for Maxillomandibular advancement (MMA) the primary surgery performed by oral and maxillofacial surgeons for sleep apnoea. In some cases, rapid maxillary widening may be considered the more suitable surgery for more information on this click here.
Pre-Surgery Preparation
- Orthodontic Treatment (if required): You may need braces or orthodontic work to align your teeth before surgery.
- Diagnostic Imaging: Cone beam X-rays, measurements, and 3D modelling of your jaws are completed.
- Surgical Planning: Using virtual surgical planning, Dr van Mourik maps out the procedure. Custom surgical plates and guides are then made.
On the Day of Surgery
- Hospital Setting: Surgery takes place in a private hospital.
- Anaesthesia: You will be put to sleep under a general anaesthetic, safely administered by a specialist anaesthetist.
During Surgery
- Incisions: Most surgery is performed inside the mouth, leaving no visible scars. Rarely, small external incisions are needed, which Dr van Mourik places within natural skin creases to minimise visibility.
- Bone Repositioning: Precise bone cuts (osteotomies) are made in the upper (maxilla) and lower jaw (mandible), and the jaws are repositioned. They are fixed securely with titanium plates and screws.
After surgery and healing
- Bone Healing: The jawbone heals over a period of 6–8 weeks.
- Plates and Screws: Titanium plates and screws remain permanently in place.
- Post-Surgical Orthodontics (if required): Minor orthodontic adjustments may be needed, usually beginning about 6 weeks after surgery.
Recovery after MMA jaw surgery for sleep aponea
Proper care after your surgery is essential for a smooth recovery. To learn about recovery after Rapid Maxillar Expanders (RME) click here.
Hospital Stay
- Double jaw surgery: 2–3 nights in hospital.
- Maxillary expansion: day surgery
- You’ll be discharged once you can eat and drink without assistance.
Pain Management
- In hospital: Pain is controlled with intravenous analgesia (pain relief), prescribed by the anaesthetist and self-administered with a button.
- After 48 hours: Most patients manage well with pain tablets such as Nurofen® or Panadeine®.
- At home: You’ll continue with oral medication, usually in liquid form. Antibiotics and other medicines may also be prescribed.
Stitches
- Dissolving stitches are used in most cases.
- They gradually disappear over 2–3 weeks without needing removal.
Elastics (for surgeries of upper and lower jaw)
- Your teeth will feel tightly closed when you wake up—this is due to orthodontic elastics.
- These support jaw healing and comfort during swelling.
- Elastics are gradually loosened over 6 weeks and removed at your 6-week check-up.
Swelling
- A head wrap with a cooling pad will be used to minimise swelling. This should stay in place for 1–2 days with fresh ice added regularly.
- Swelling usually peaks around day 3–4 and then gradually improves.
- Keep your head elevated (2–3 pillows or a recliner) for about a week.
- It may take several weeks for swelling to completely resolve.
Bleeding & Bruising
- Mild oozing in the mouth or nose is normal.
- Large clots may be dislodged occasionally. If any heavy, bright red bleeding contact us.
- Bruising is very common after lower jaw surgery and may extend down the neck and chest.
Diet
- Upper and lower jaw surgery: A soft diet is required for 5-6 weeks.
- Some weight loss is common, frequent high-protein, high-calorie meals will help aid recovery.
Oral Care
- Begin gentle brushing with a soft, child’s toothbrush as soon as possible.
- Rinse with warm saltwater (1 tsp salt in 1 glass of warm water) at least 3 times daily.
Returning to Work, School & Exercise
- MMA: 2–3 weeks off
- Most patients feel better after 2 weeks, but full energy may take 6 weeks.
- Avoid strenuous exercise until fully recovered.
- No contact sports for 3 months.
- Maxillary expansion devices: About 1 day off.
Recovery Timeline
- Bone healing: 6–8 weeks.
- Full recovery for larger lower and top jaw surgeries : 3–6 months.
- Post-surgical orthodontics (if needed): May begin about 6 weeks after surgery.
Follow-Up Care
- Dr van Mourik will want to see you periodically to monitor your healing and ensure that your jaws are staying properly aligned..
- Further check-ups at 6 months and 12 months to monitor healing and jaw alignment.
- Atten ding these appointments is crucial for long-term success.
Important Notes
- Do not blow your nose for 2 weeks if you had upper jaw or nasal surgery.
- Use saline spray and prescribed decongestants as directed.
- Report swelling or pain in one leg immediately, as this may signal a blood clot.
Dr van Mourik will provide you with tailored post-operative instructions before your surgery. Please follow them closely to maximise healing and minimise complications.
Benefits of OSA surgery
Obstructive sleep apnoea can seriously impact your sleep quality, daily performance, and long-term health. Surgery may be recommended when other treatments haven’t worked, offering benefits such as:
- Better quality sleep – reduces airway blockages that cause repeated awakenings.
- More energy during the day – lowers daytime sleepiness and fatigue.
- Reduced snoring – improving sleep for both you and your partner.
- Improved concentration and mood – fewer interruptions to sleep helps restore focus and mental clarity.
- Lower health risks – decreases spikes in blood pressure, reducing risk of heart attack, stroke, and depression.
- Relief from discomfort – fewer morning headaches, dry mouth, and sore throat.
By addressing the root cause of airway obstruction, OSA surgery can help restore healthy breathing during sleep and improve your overall quality of life.
A Personalised Approach
Corrective jaw (orthognathic) surgery is never “one-size-fits-all.” Treatment is carefully planned based on your unique facial structure, bite, and concerns. Beyond restoring functional bite alignment, it also enhances appearance by balancing the proportions of the teeth, chin, and facial profile. The result is not only better oral health, but also a more natural and harmonious facial appearance—both from the front and side views.
Obstructive Sleep Aponea Jaw Surgery in Sydney Costs NSW
The cost of corrective jaw surgery depends on the type of procedure, hospital requirements, and anaesthesia.
- Medicare provides a rebate for part of the consultation and certain surgical item numbers.
- A written, itemised quote is given before treatment, which can be submitted to your private health fund to confirm any rebates.
- Private health insurance may cover part of the hospital admission and anaesthetist’s fees.
Patients are encouraged to check both Medicare and private health fund entitlements prior to surgery so that they are fully informed about expected costs.
Meet Dr Kristian van Mourik
Dr Kristian van Mourik is a fully qualified Oral & Maxillofacial Surgeon with more than 15 years of specialist practice in Sydney. He holds dual degrees in medicine and dentistry, supported by extensive surgical training, making him one of the few surgeons in Australia with this level of expertise.
Academic background includes:
- Bachelor of Biomedicine – Monash University
- Bachelor of Dentistry with Honours – University of Sydney
- Bachelor of Medicine / Bachelor of Surgery – University of Sydney
His practice covers the full scope of oral and maxillofacial surgery, including TMJ disorders, corrective jaw surgery, wisdom tooth removal, dental implants, trauma surgery, and oral pathology. Dr van Mourik is registered with both the Medical Board of Australia and the Dental Board of Australia as a specialist Oral & Maxillofacial Surgeon.
Areas We Service for Sleep Apnoea Surgery
Sleep apnoea surgery and treatment are available across Sydney’s Eastern Suburbs and North Shore. Dr Kristian van Mourik provides specialist surgical care for patients experiencing obstructive sleep apnoea, snoring, or airway obstruction at our Bondi Junction and Lindfield clinics.
- Bondi
- Bronte
- Clovelly
- Coogee
- Randwick
- Paddington
- Woollahra
- Double Bay
- Bellevue Hill
- Tamarama
- Waverley
- Surrounding Eastern Suburbs
- Roseville
- Chatswood
- Killara
- Gordon
- Pymble
- Turramurra
- St Ives
- Wahroonga
- Hornsby
- Willoughby
- Castle Cove
- Other North Shore suburbs
OSA surgery FAQS
Do I have sleep aponea?
Most symptoms of obstructive sleep apnoea (OSA) happen while you’re asleep, which can make it difficult to recognise the condition on your own. Often, it’s a partner who first notices the signs. If you feel tired during the day despite a full night’s sleep, or find your rest frequently disrupted, OSA may be the cause. Other common symptoms include loud snoring, morning jaw pain, teeth grinding, headaches, and waking up short of breath.
If you recognise these signs, we recommend booking a consultation to see whether sleep apnoea surgery in Sydney could be an option for you.
Is sleep aponea genetic?
Obstructive sleep apnoea in adults is often linked to excess weight, while in children, common causes include enlarged tonsils or orthodontic issues. The condition can also be influenced by hereditary anatomical features, such as a thick neck, narrow throat, or round head shape. If you have a family history of sleep apnoea and experience symptoms like loud snoring, daytime fatigue, or low energy, these inherited traits may increase your risk.
We recommend that you see Dr Van Mourik in consultation with your sleep specialist to determine whether you qualify for sleep apnoea surgery in Sydney.
Is sleep aponea dangerous?
If left untreated, obstructive sleep apnoea can contribute to serious health issues such as high blood pressure, diabetes, stroke, and heart disease, making it a significant medical concern. Beyond these risks, it can also affect daily life — leading to reduced performance at work, underachievement and behavioural problems in children, and worsening conditions such as ADHD or depression due to poor sleep and daytime fatigue. We strongly recommend seeking proper diagnosis and treatment. This may include a consultation with Dr Van Mourik, who will work alongside your sleep specialist to determine if you could benefit from sleep apnoea surgery in Sydney.
Is sleep apnoea surgery covered by medicare?
Some Medicare item numbers may apply to hospital and anaesthetist costs. We provide a detailed written quote before treatment. We recommend you check with your private health insurer to confirm your coverage. For affordable sleep aponea surgery in Sydney, Dr van Mourik can guide you through your options.
Is sleep apnoa surgery covered by private health insurance?
Private health insurance can contribute to hospital, surgeon’s and anaesthetist’s fees. We provide a detailed written quote before treatment. We recommend you check with your private health insurer to confirm your coverage. For affordable sleep aponea surgery in Sydney, Dr van Mourik can guide you through your options.
Do I need sleep aponea surgery?
Not everyone with obstructive sleep apnoea (OSA) needs surgery. For most people, the first line of treatment is CPAP or an oral appliance. Surgery may be an option if:
- You’ve tried CPAP or an oral device but found them difficult to tolerate.
- You have physical factors such as enlarged tonsils, nasal blockages, or jaw alignment issues.
- Your symptoms continue even after trying other treatments.
For an expert opinion, Dr van Mourik is considered one of the best sleep aponea surgeon in Sydney.
Our Sydney Clinics

Bondi Junction
Located in the heart of the Eastern Suburbs, our Bondi Junction clinic is easily accessible by train, bus, and nearby parking.

Lindfield
Conveniently positioned on the North Shore, our Lindfield clinic is close to public transport and offers parking options nearby.
