Specialist care for facial trauma in Sydney
Facial Trauma Sydney
Facial trauma can result from accidents, sporting injuries, falls, or assaults. In some cases, disease or infection may weaken the bones of the face and increase the risk of fracture. Injuries of this kind need careful assessment, as undetected or untreated fractures can affect function, healing, and appearance over time.
Facial trauma Surgery in Sydney
Specialist oral surgery practice with over 15 years’ experience, two Sydney clinics, and a commitment to safe, evidence-based care.


With over 15 years of specialist experience, Dr Kristian van Mourik provides surgical and non-surgical management of facial trauma at clinics in Bondi Junction and Lindfield. Supported by advanced imaging, hospital-grade facilities, and evidence-based techniques, care is focused on restoring function and supporting safe healing.
Dr Kristian Van Mourik Associations & Accreditations







What Are Facial Fractures?
Facial fractures, also called Maxillofacial Tauma, occur when one or more of the bones in the face are broken. Facial bones are relatively thin and delicate, making them vulnerable to fractures. This type of injury can be caused by motor vehicle accident, a physical assault, sporting injury or al fall. Occasionally disease or infection can weaken facial bones leading to a fracture.
Types of Facial Injuries Treated
Facial trauma can affect one or multiple bones of the face. Each type of fracture presents differently and requires individual assessment to decide whether observation or surgery is appropriate.
Cheekbone (zygoma) fractures
The zygoma, or cheekbone, plays a key role in facial width and contour. A fracture can flatten the cheek, alter facial balance, and restrict jaw movement. In some cases, patients may notice changes in vision if the fracture extends into the orbital rim. Surgical repair may be recommended to restore symmetry and prevent long-term functional problems.
Upper jaw (maxilla) fractures
The maxilla is central to the bite and midface structure. Fractures here can destabilise the teeth, affect how the upper and lower teeth meet, and sometimes involve the nasal cavity or eye sockets. Treatment often involves careful reconstruction to restore bite function and facial support.
Lower jaw (mandible) fractures
The mandible is the most commonly fractured facial bone. Injuries may cause pain, swelling, bruising, and difficulty opening or closing the mouth. Depending on the location and displacement, repair may require plates and screws to stabilise the fracture and protect the bite.
Nasal fractures
Nasal injuries are frequent in sports, falls, and assaults. A broken nose can affect both breathing and appearance. Early assessment helps determine whether manipulation or surgical intervention is required to restore airflow and nasal alignment.
Frontal sinus fractures
Located above the eyes, the frontal sinuses can be fractured in high-impact trauma such as motor vehicle accidents. These injuries may extend into surrounding structures and often require more complex surgical management. Specialist care is essential to protect both function and appearance.
Orbital fractures
Fractures of the orbit, or eye socket, can affect vision, eye position, and facial symmetry. Symptoms may include double vision or restricted eye movement. Depending on severity, surgical repair may involve repositioning bone fragments and supporting the orbital floor to protect the eye.
How Do I Know If I Have Broken a Bone in My Face?
The symptoms of a facial fracture vary depending on which part of the face has been injured.
General signs of a facial fracture can include:
- Swelling and bruising
- Pain or tenderness around the affected area
- Numbness or tingling in the face
- Visible deformity or asymmetry
Nasal fractures (broken nose) may cause:
- Difficulty breathing through the nose
- Nosebleeds
- Changes to the shape or alignment of the nose
Jaw fractures (maxillary or mandibular) may present with:
- Pain when opening or closing the mouth
- Difficulty chewing, swallowing, or speaking
- Drooling due to restricted movement
- Loose, broken, or missing teeth
- s
Orbital fractures (eye socket injuries) may lead to:
- Blurred or double vision
- Bulging or sunken appearance of the eye
- Difficulty moving the eye in certain directions
If you experience any of these symptoms after an injury, it’s important to seek prompt assessment by an Oral and Maxillofacial Surgeon to ensure accurate diagnosis and proper treatment.
Problems Caused by Facial Fractures
Facial bone fractures can affect both appearance and function. Depending on the area of injury, you may experience difficulties with everyday activities — for example, a jaw fracture can make eating painful, while a nasal fracture can cause breathing problems.
In addition to these functional issues, facial trauma can sometimes lead to more serious complications such as infection, internal bleeding, or nerve and brain-related concerns.
Seeking prompt assessment and treatment from an Oral and Maxillofacial Surgeon after facial trauma is essential to minimise complications and ensure the best possible recovery.

How are Facial Fractures Diagnosed?
Facial fractures are diagnosed through a combination of physical examination and imaging tests.
During your consultation, the Oral and Maxillofacial Surgeon will first assess your overall condition to ensure there are no life-threatening injuries. They will then carefully examine your face for swelling, bruising, deformity, or tenderness, and gently press on the facial bones to determine the extent of injury.
Additional checks may include:
- Assessing vision and eye movement
- Checking nasal passages and airways for obstruction
- Evaluating bite alignment (occlusion) to identify possible jaw fractures
- Testing for signs of head or spinal injury
Imaging tests are used to confirm the type, location, and severity of the fracture:
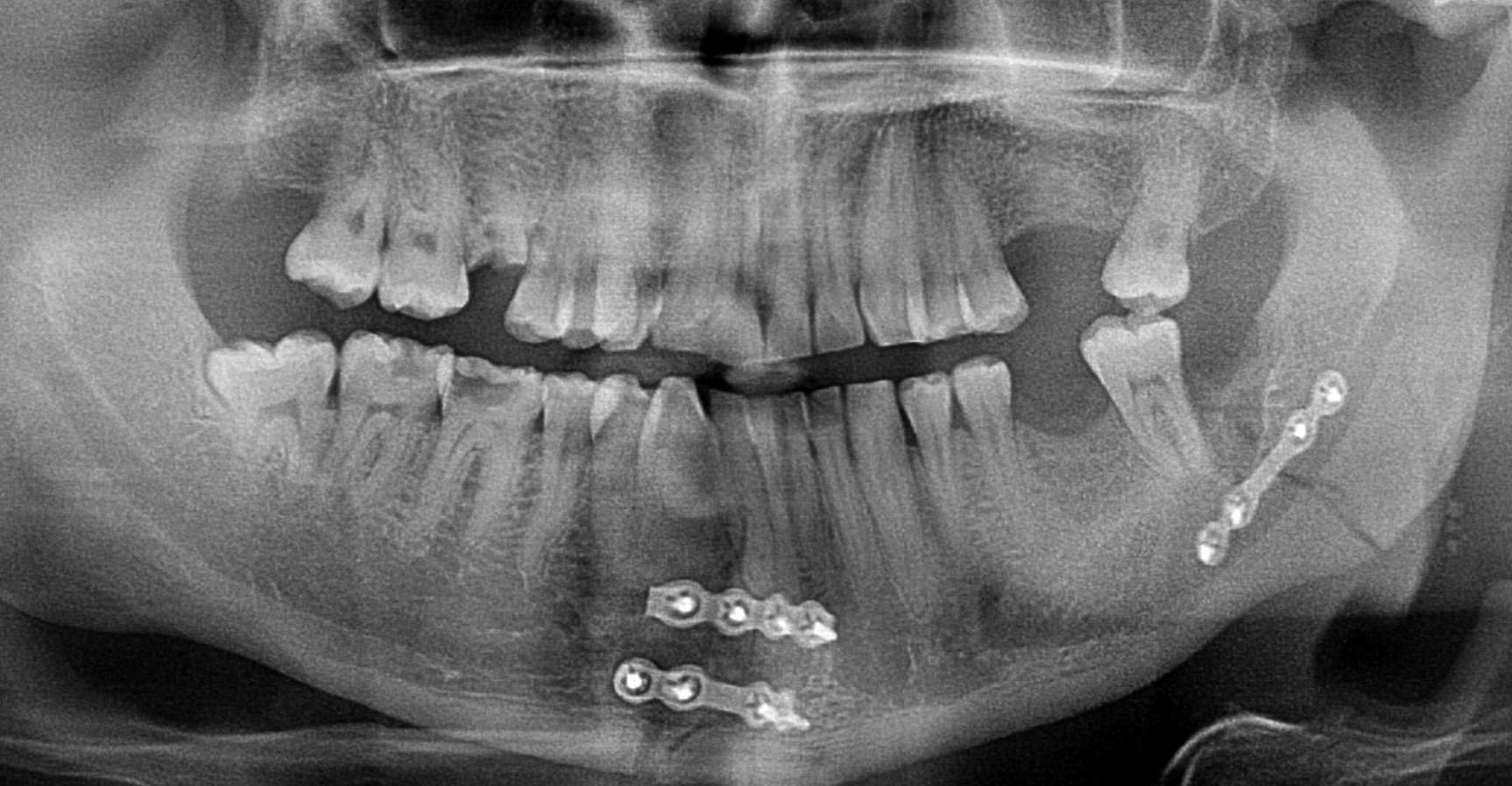
- CT scans – the most accurate and commonly used method, providing detailed images of bones, soft tissues, and blood vessels
- X-rays – useful for examining bones, they are less detailed than a CT scan but helpful for nasal or jaw fractures. This thorough assessment ensures an accurate diagnosis and helps guide the most appropriate treatment plan for each patient.
Treatment and surgery for facial fractures
Treatment for facial fractures depends on where the injury is, how severe it is, and which neighbouring organs such as your eye or brain may be involved. The main goal is to restore your normal appearance, prevent infection and restore function including breathing, speaking and chewing.
Initial Care After a Facial Injury
Early care may involve:
- Controlling bleeding with gentle pressure
- Reducing swelling by keeping your head elevated and applying ice packs
- Managing pain with prescribed pain relief
- Preventing infection with antibiotics, if needed
Non-Surgical Treatment
Not all facial fractures require surgery. Some mild fractures can heal naturally with careful monitoring. In these cases, your surgeon may recommend:
- Closed reduction – gently moving the bones back into place without surgery
- Pain and swelling management with medication and rest
- A soft diet and limiting jaw movement while healing takes place
Surgical Treatment
Surgery under general anaesthesia in a hospital is often needed if the bones are displaced, unstable, or affecting important functions like chewing, breathing, or vision. Depending on the type of fracture, surgery will be performed immediately or delayed a few days until swelling settles.
Common surgical treatments include:
- Open Reduction and Internal Fixation (ORIF): The most common procedure, where titanium plates and screws are used to hold the bones in place.
- Jaw wiring: In some jaw fractures, the upper and lower jaws may be temporarily wired together to keep them stable during healing.
- Reconstructive surgery: For complex or multiple fractures, reconstructive surgery may be required to restore facial shape and function.
Recovery After a Facial Fracture
Recovery from a facial fracture varies from person to person and depends on the severity of the injury, the type of treatment you’ve had, and your general health. Most people recover well in few months, but complete healing can take 4-6 months.
What to Expect After Surgery
Most people who undergo facial fracture or reconstructive surgery notice that swelling and bruising improve within about two weeks, though it can take a few months for full recovery.
- Hospital Stay: Most patients stay in hospital for one to two days after surgery.
- Pain Management: While in hospital, you’ll receive intravenous pain relief prescribed by your anaesthetist, which you can self-administer if needed. Within about 48 hours, most people can comfortably switch to oral pain medication such as Nurofen® or Panadeine Forte®.
- Work or School: You’ll usually need about a week off work or study, though this may vary depending on the extent of your fracture.
- Stitches: Dissolving stitches are typically used and will gradually disappear over three to four weeks.
- Diet: After a jaw fracture, you’ll need to follow a soft diet for four to six weeks to allow proper healing.
- Follow-Up Appointments: Dr van Mourik will schedule regular reviews to monitor your recovery and ensure everything is healing as expected.
Why See an Oral & Maxillofacial Surgeon?
Oral and Maxillofacial Surgeons are specialists trained in medicine, dentistry, and surgery. This combination of expertise allows them to:
- Manage the full range of facial fractures, from simple to complex
- Provide both non-surgical and surgical treatment options depending on the injury
- Perform procedures in accredited hospitals with specialist anaesthetists
- Plan and perform surgery using advanced imaging and recognised surgical techniques
- Coordinate care when medical conditions or multiple injuries are involved
Meet Dr Kristian van Mourik
Meet Dr Kristian van Mourik
Dr Kristian van Mourik is a fully qualified Oral & Maxillofacial Surgeon with dual qualifications in medicine and dentistry, as well as specialist surgical training. He has more than 15 years’ experience managing facial trauma, corrective jaw surgery, wisdom tooth removal, dental implants, and oral pathology.
Qualifications include:
- Bachelor of Biomedicine – Monash University
- Bachelor of Dentistry with Honours – University of Sydney
- Bachelor of Medicine / Bachelor of Surgery – University of Sydney
Dr van Mourik is registered with both the Medical Board of Australia and the Dental Board of Australia as a specialist Oral & Maxillofacial Surgeon.
Sydney Suburbs We Service for Facial Trauma
Facial trauma assessment and treatment is available across Sydney’s Eastern Suburbs and North Shore.
- Bondi
- Bronte
- Clovelly
- Coogee
- Randwick
- Paddington
- Woollahra
- Double Bay
- Bellevue Hill
- Tamarama
- Waverley
- Surrounding Eastern Suburbs
- Roseville
- Chatswood
- Killara
- Gordon
- Pymble
- Turramurra
- St Ives
- Wahroonga
- Hornsby
- Willoughby
- Castle Cove
- Other North Shore suburbs
Facial Trauma FAQs Sydney
Do all facial fractures require surgery?
No. Many minor or non-displaced fractures heal without an operation. Regular reviews and imaging are used to monitor progress.
How soon should a facial fracture be treated?
If surgery is required, it is often performed within the first week after injury once swelling decreases. Timing is tailored to each case.
Will plates and screws need to be removed?
Plates and screws used to stabilise fractures are usually permanent. Removal is only considered if they cause problems later on.
How long does recovery take after facial fracture surgery?
Swelling and bruising generally improve within two weeks. Most patients return to work or school within one to two weeks. Complete bone healing takes several months.
Where is facial trauma surgery performed in Sydney?
Procedures are carried out in accredited private hospitals, with anaesthesia provided by specialist anaesthetists and follow-up arranged through Dr van Mourik’s Bondi Junction and Lindfield clinics.
Do Sydney patients need time off work or school after wisdom tooth extraction?
Most people need about a week away from regular activities. Teenagers often schedule surgery during school holidays, while university students and young professionals choose quieter times in their schedule to allow recovery. The amount of time required depends on the complexity of surgery and individual healing.
Is wisdom tooth removal different in Sydney compared to other areas?
The procedure itself is the same, but Sydney patients benefit from access to Oral & Maxillofacial Surgeons who regularly perform complex extractions in hospital and clinical settings. Having two clinics one in Bondi Junction and one in Lindfield — provides convenient access for patients across the Eastern Suburbs and North Shore.
Our Sydney Clinics

Bondi Junction
Located in the heart of the Eastern Suburbs, our Bondi Junction clinic is easily accessible by train, bus, and nearby parking.

Lindfield
Conveniently positioned on the North Shore, our Lindfield clinic is close to public transport and offers parking options nearby.
